

Written by Clinical Lead Dr Ambi Sud
And Qr8 PhD Candidate Aoibhe Mulcahy
Retinol products have become essential components in skincare routines, celebrated for addressing concerns like acne, fine lines, texture and congestion, and uneven skin tone.
In Australia, these Vitamin A derivatives are among the most sought-after skincare ingredients, reflecting their widespread popularity among consumers.
Here’s a deep dive on what they are, how they work, and which forms of retinol are the most effective.
What is Retinol?
Retinol is an umbrella term for all forms of Vitamin A, including those used topically on the skin. This includes the synthetic retinoids and their derivatives (e.g. tretinoin, tazarotene, adapalene), retinaldehyde (retinal), retinoic acid esters (hydroxypinocacolone retinoate, retinyl retinoate) & the retinyl esters (retinyl palmitate, retinyl acetate, retinyl propionate).
The terminology used in practice is slightly different, however: RETINOLS normally include cosmetic (over-the-counter) products that don’t require a doctor’s written prescription, whilst RETINOIDS are those forms of retinol that need a prescription.
This post primarily relates to prescription-strength retinoids as the scientific evidence is strongest for their actions in the skin, and it’s the form of retinoids our doctors prescribe if appropriate for the patient. For example, the prescription retinoid tretinoin is 20x stronger than a cosmetic retinol.
Topical Retinol Strengths Explained
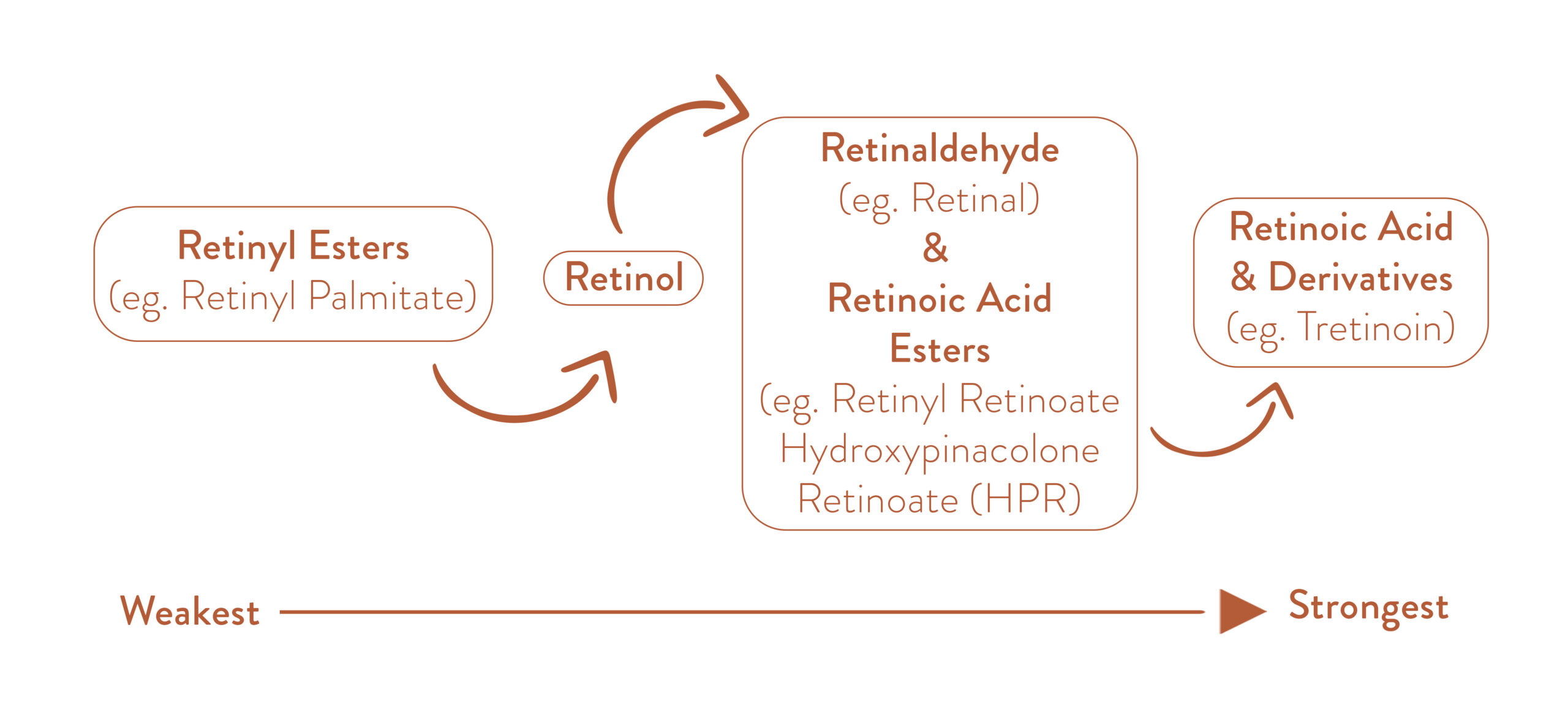
Retinyl esters are the weakest form of retinol and retinoic acid (and its derivatives) is the strongest, which is why it needs a prescription.
In order to work in the skin, there is a multi-step pathway, during which less potent forms of retinol are converted to the active forms – the diagram below explains this process and rates the different retinoids on a scale from weakest to strongest:
What Do Retinoids Do For Your Skin?
The scientific literature shows that topical retinoic acid:
- Increases skin cell turnover (it’s like internal exfoliation!)
- Plumps the dermis by increasing collagen and elastin production, blocking enzymes that break down collagen, and increasing the activity of the cells that produce collagen, elastin and hyaluronic acid.
- Fades pigmentation and speeding up removal of pigmented skin cells
- Stimulates growth of new blood vessels deep in the skin (these are different to ‘broken capillaries’ that are visible in the skin)
- Increases the skin’s hyaluronic acid (HA) production by increasing activity of the cells that produce HA in the skin
What Skin Conditions Can Retinoids Treat?
- Signs of ageing including sun damage and fine lines (they are considered the ‘gold standard’ for this!)
- Acne / oily skin
- Rosacea – however this is with caution, as their role is in long-term management / control of rosacea, rather than to control an acute flare. We have other ingredients than can be of benefit at this time, such as OXYMETAZOLINE, and work well with retinoids once a flare has been treated adequately
- Melasma / pigmentation (in conjunction with other pigment-fading ingredients)
NOTE: There is a lack of evidence from properly designed clinical trials to support the claimed efficacy of cosmetic retinoids for anti-aging.
How Do the Types of Retinoids Differ?
Over-the-counter Retinoids
These include retinyl esters, retinol, retinaldehydes and the retinoic acid esters. They are less potent than their prescription counterparts, and may not provide dramatic outcomes, especially for treatment of skin conditions such as acne and pigmentation. They are applied directly to the skin surface (topically).
Prescription Retinoids
These include the synthetic retinoids tretinoin, tazarotene and adapalene (along with others such as trifarotene which aren’t available in Australia) which all require a prescription from a doctor. The benefit of prescription retinoids is that they are already active, so do not be converted into an active form like over-the-counter retinoids to work on the skin. Like over-the-counter formulations, they are applied to the skin surface, and can also be combined with various other ingredients to make them more targeted towards particular skin concerns.
Systemic Retinoids
This includes isotretinoin (trade names: Roaccutane, Accutane, Oratane) – a drug commonly used in the treatment of severe cystic acne and rosacea. It can only be prescribed by a dermatologist, and not by other medical practitioners, such as GPs. It is taken orally, and works differently from topical formulas and primarily targets oil glands in the skin by shrinking them and reducing oil production. The Therapeutic Goods Association has just released new 2025 safety warnings regarding mental and sexual health when using isotretinoin. Read more HERE.
Common Side Effects of Topical Retinoids
When retinoids are being introduced to the skin, the following may occur (and are more likely with potent prescription retinoids, which is why expert management is essential):
- Peeling – this should never be more than light ‘face dandruff’ and without associated inflammation
- Purging – this can be especially frustrating when the initial problem of acne seems to worsen, but is a sign the retinoid is working the way it’s meant to. It doesn’t happen to everyone and isn’t as common as the internet would have you believe!
- Redness – this should not be bumpy, irritated or sore
- Slight stinging, tingling or warmth on application
- Dryness
With a phased introduction plan and the right supporting skincare, these symptoms can be managed to almost no symptoms at all. With time and consistency (rather than stopping and starting – which can be tempting to do when experiencing side effects!), your skin adjusts and these symptoms resolve.
Like any drug, there is a spectrum when it comes to side effects for all kinds of reasons, and our expert Support Team help you tolerate your treatment so you can use it daily as prescribed.
Are You Using the Right Retinoid Dose?
0.025% tretinoin is the lowest dose for a multitude of skin conditions (like acne) with scientific evidence behind it.
Increased doses of 0.05% and even 0.1% can be prescribed, although come with greater chance of side effects.
A 0.01% dose can be useful for patients who are easing themselves into prescription retinoids, that have poorly tolerated higher doses, or want a bit of a ‘glow’ with less chance of side effects.
Tazarotene is prescribed at a concentrations of 0.05% – 0.1% in topical treatments.
Adapalene is available in strengths from 0.1 – 0.3% in prescription treatments.
When it comes to retinoids, there is no absolute ‘right strength’ – will be different for everyone, and something that should be personalised to you and your skin condition. For anti-aging/sun damage, you want to aim for the dose that you can tolerate daily without side effects – stronger isn’t always better!
COMMON RETINOID MYTHS
It’s a common belief that retinoids make you more sensitive to the sun, and therefore more likely to get sunburnt. For this reason, many fear to use a retinoid during warmer months and cease their treatment during summer or when going on a sunny holiday.
Read the science behind why this is a myth HERE.
This is one myth that just won’t disappear! Retinoid use actually thickens the dermis through additional collagen, elastin and hyaluronic acid production.
We break down this myth HERE!
Yep, another myth, we bust HERE!
The ‘best’ time to start a retinoid it’s not *actually* about your chronological age.
Read more about this myth HERE.
How long do retinoids take to work?
This will vary patient-to-patient, and depends on what condition is being treated, its severity and if you are following your supporting skincare advice (including… you’ve guessed it… your sunscreen!).
Are Retinoids Safe for Long-Term Use? Here’s What the Science Says
Prescription retinoids, like tretinoin, have been trusted by dermatologists for over 50 years. Even though newer options like tazarotene exist, tretinoin remains one of the most researched and reliable treatments.
In a 2005 study, skin treated with tretinoin for 12 months (most clinical studies are for 3 months) showed no damage under the microscope. Skin cells stayed healthy, and elastic tissue remained intact.
Another long-term study found that using tretinoin for 4 years (considered a lifetime in scientific studies!) actually thickened the dermis — the deeper layer of skin. This is what helps smooth out fine lines and wrinkles.
Most of these changes take at least 6 months of regular (daily) use, with even more visible improvements the longer you use it. Over time, skin texture, wrinkles, and pigmentation all improve.
Tretinoin isn’t just safe — it’s essential for maintaining results from acne, pigmentation, and even rosacea treatments.
So, are retinoids safe long-term? The evidence says yes.
WE SEE YOU. WE UNDERSTAND YOUR FRUSTRATION WITH FINDING SOLUTIONS FOR MELASMA, ACNE, SUN DAMAGE, ROSACEA AND PIGMENTATION.
WE’RE HERE TO HELP.
BOOK A CONSULTATION WITH AN EXPERIENCED AUSTRALIAN DOCTOR TODAY TO DISCUSS YOUR SKIN TREATMENT OPTIONS: CLICK HERE
REFERENCES:
Spierings NMK. Evidence for the Efficacy of Over-the-counter Vitamin A Cosmetic Products in the Improvement of Facial Skin Aging: A Systematic Review. J Clin Aesthet Dermatol. 2021 Sep;14(9):33-40. PMID: 34980969; PMCID: PMC8675340.
Karadag, A.S., Aksoy, B., & Parish, L.C. (Eds.). (2019). Retinoids in Dermatology (1st ed.). CRC Press. https://doi.org/10.1201/9780429456732
Baldwin HE, Nighland M, Kendall C, Mays DA, Grossman R, Newburger J. 40 years of topical tretinoin use in review. J Drugs Dermatol. 2013 Jun 1;12(6):638-42. PMID: 23839179.
Anzengruber F, Czernielewski J, Conrad C et al. Swiss S1 guideline for the treatment of rosacea. J Eur Acad Dermatol Venereol. 2017;31:1775–1791.
Reinholz M, Tietze JK, Kilian K et al. Rosacea – S1 guideline. J Dtsch Dermatol Ges. 2013;11:768–780
Kang S, Bergfeld W, Gottlieb AB, Hickman J, Humeniuk J, Kempers S, Lebwohl M, Lowe N, McMichael A, Milbauer J, Phillips T, Powers J, Rodriguez D, Savin R, Shavin J, Sherer D, Silvis N, Weinstein R, Weiss J, Hammerberg C, Fisher GJ, Nighland M, Grossman R, Nyirady J. Long-term efficacy and safety of tretinoin emollient cream 0.05% in the treatment of photodamaged facial skin: a two-year, randomized, placebo-controlled trial. Am J Clin Dermatol. 2005;6(4):245-53. doi: 10.2165/00128071-200506040-00005. PMID: 16060712.
Bhawan J, Olsen E, Lufrano L, Thorne EG, Schwab B, Gilchrest BA. Histologic evaluation of the long term effects of tretinoin on photodamaged skin. J Dermatol Sci. 1996 Mar;11(3):177-82. doi: 10.1016/0923-1811(95)00432-7. PMID: 8785167.
Yamamoto O, Bhawan J, Solares G, Tsay AW, Gilchrest BA. Ultrastructural effects of topical tretinoin on dermo-epidermal junction and papillary dermis in photodamaged skin. A controlled study. Exp Dermatol. 1995 Jun;4(3):146-54. doi: 10.1111/j.1600-0625.1995.tb00238.x. PMID: 7551562.
Mambwe B, Mellody KT, Kiss O, O’Connor C, Bell M, Watson REB, Langton AK. Cosmetic retinoid use in photoaged skin: A review of the compounds, their use and mechanisms of action. Int J Cosmet Sci. 2025 Feb;47(1):45-57. doi: 10.1111/ics.13013
Milosheska D, Roškar R. Use of retinoids in topical antiaging treatments: a focused review of clinical evidence for conventional and nanoformulations. Adv Ther. 2022;39(12):5351–5375.
Darlenski R, Surber C, Fluhr JW. Topical retinoids in the management of photodamaged skin: from theory to evidence-based practical approach. Br J Dermatol. 2010;163(6):1157–1165.




















