

Written by PhD Candidate Aiobhe Mulcahy
Fact Checked by Dr Ambi Sud
If you have melasma, you know how deeply frustrating it can be. The persistent, patchy brown pigmentation isn’t just a skin condition—it can impact your confidence, your emotional well-being, and even how you feel about stepping outside without makeup.
It’s no surprise that people are searching for answers. Some claim that poor gut health and metabolic syndrome – a cluster of conditions like insulin resistance, obesity, and chronic inflammation – causes melasma and that you can ‘cure’ it with diet, gut health supplements, and gut health foods.
But here’s the truth: Science doesn’t support this claim.
At Qr8 our teledermatology clinic in Australia, we see and treat people with melasma every day. We understand how distressing it can be, especially in our harsh Australian climate, where intense UV exposure makes pigmentation harder to manage. But with the right evidence-based approach, you can take control of melasma all year round and feel more confident in your skin.
What is Melasma?
Melasma is a chronic pigmentary disorder that causes dark patches on sun-exposed areas, typically the face, neck, chest, and arms. It’s most common in women, people with darker skin tones, and those with a family history of the condition.
Unlike freckles or sunspots, melasma often – but not always – appears in symmetrical patterns, most commonly on the forehead, cheeks, nose, chin, and upper lip (the dreaded sun-stache). It can be unpredictable – fading with treatment, only to return after sun exposure or hormonal changes.
In Australia, where UV radiation levels are among the highest in the world, managing melasma is particularly frustrating. Many people find that their melasma worsens in summer and improves slightly in winter – but without proper treatment, it often persists year-round, and worsens over time.
Why are chemical peels NOT the best melasma treatment?
What Causes Melasma?
Melasma isn’t fully understood, but research has identified four key triggers. These are the proven causes of melasma:
✅ Sun exposure – The #1 melasma trigger. UV radiation stimulates pigment-producing cells (melanocytes), leading to excess pigment. Even visible light – especially blue light from the sun (not your phone, iPad, computer!) – can worsen melasma, which is why pigmentation often returns, even with diligent sun protection.
✅ Hormonal changes – Pregnancy, birth control pills, and hormone therapy can all trigger melasma by increasing estrogen levels, which stimulate melanin production.
✅ Genetics – Some people are simply more prone to melasma. It runs in families and affects both men and women.
✅ Certain medications – Birth control pills, antibiotics, and anti-seizure drugs can increase skin’s sensitivity to sunlight, making melasma worse.
❌ What’s NOT a proven cause of melasma?
Blood sugar levels, inflammation, obesity, poor gut health, and other metabolic factors!
What Is Metabolic Syndrome?
Metabolic syndrome is a systemic health condition linked to heart disease and diabetes. The presence of any three of the following five risk factors is diagnostic of Metabolic Syndrome:
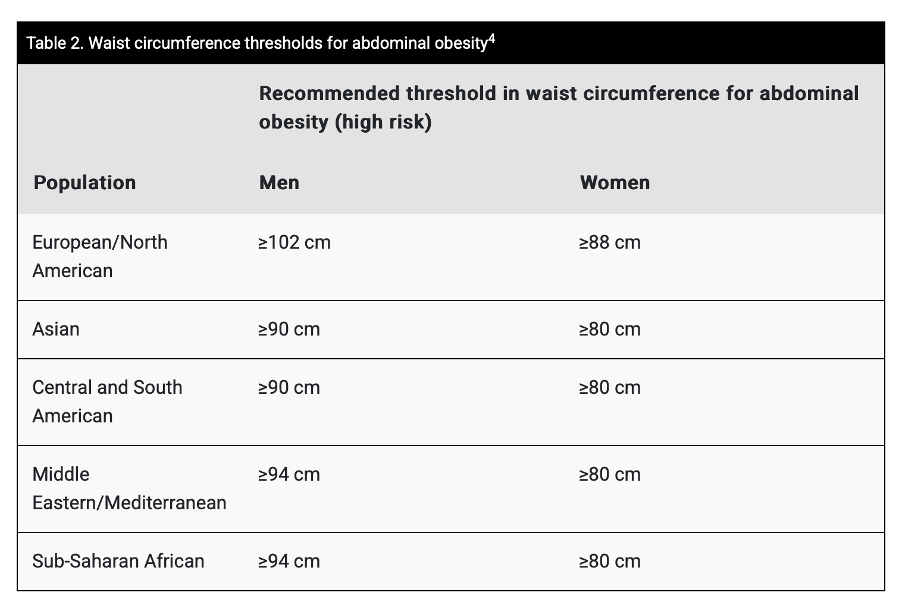
✔ Waist Measurement (differs for different ethnic groups, see table below)
✔ High blood pressure (>130/85 mmHg)
✔ High blood sugar (>5.6 mmol/L)
✔ High triglycerides (>1.7 mmol/L)
✔ Low HDL (‘good’) cholesterol (<1.0 mmol/L for men, <1.3 mmol/L for women)
Does Science Support a Melasma-Metabolic Syndrome Link?
We understand why so many people want to believe that melasma is connected to diet or metabolic health – because that would mean there’s a simple, controllable way to fix it. But despite the claims, scientific research just doesn’t support this theory.
Several studies have attempted to connect metabolic syndrome to melasma, but the evidence is weak. Here’s why:
1️. A study found higher insulin resistance in melasma patients, but the study had major flaws: a small sample size (only 50 cases, 44 controls), failure to account for lifestyle and sun exposure, and statistically insignificant results. The study was later retracted due to unreliable findings (Karaali, 2022).
2️. Another study found metabolic abnormalities in melasma patients but failed to consider key factors like hormonal fluctuations and UV exposure. The study’s inconsistent findings weaken its credibility (Zhang et al., 2024).
3️. A third critical review of these studies highlighted these flawed methodologies, misleading study designs, and lack of proper control groups – concluding that melasma is NOT a metabolic disorder (D’Elia et al., 2022).
So, while managing metabolic syndrome is important for overall health, there’s no strong scientific evidence linking it to melasma.
This is why treating melasma with diets and supplements is a waste of time & money.
The REAL Science: What Actually Triggers Melasma?
1️. Hormonal Fluctuations & Pregnancy:
- 89.1% of melasma patients had abnormal estrogen levels compared to controls (Mahmood et al., 2016).
- 29% of women on oral contraceptives developed melasma (Resnik, 1967).
- Pregnancy-related melasma rates vary worldwide but are higher than the general public:
- 37% of pregnant women in Melbourne reported melasma (The Royal Australian College of General Practitioners, 2024)
- 46% of pregnant women in Pakistan (Handel et al., 2014)
- 6% of pregnant women in Iran (Moin et al., 2006)
2️. Sun Exposure (Both UV & Visible Light):
- 80% of melasma patients report worsening pigmentation in summer – even though they usually choose to treat it only in winter! (Liu & Fu, 2009).
- A randomized controlled trial found that broad-spectrum sunscreen significantly reduces melasma severity (Castanedo-Cazares et al., 2014).
What’s the BEST sunscreen for Melasma?
Melasma Treatment That Actually Works:
🌟 The first line treatment is a tinted sunscreen (SPF 50+)
- This is the first-line and gold standard treatment for melasma, and a non-negotiable
- Tinted sunscreen and other sun protection measures are essential for Australia’s high UV environment
- The right UV filters are essential to protect against UVA, UVB and especially UVA-1 light – and not all sunscreens contain the right filters!
🌟 Plus a Prescription Triple Combination Cream (this is considered the gold standard of melasma treatment)
- This contains hydroquinone, tretinoin, and an anti-inflammatory
- Available only through a dermatologist or prescription in Australia
🌟 Other proven second-line treatments are used to maintain skin between fading treatments:
✔ Topicals: Azelaic acid, kojic acid, arbutin, niacinamide, tranexamic acid
✔ Oral medications: Prescription tranexamic acid can help with stubborn melasma
✔ Certain Lasers: Pico, Fraxel, and Q-Switch lasers (but NOT BBL or IPL!)
Melasma may be stubborn, but with the right approach, you can manage it effectively and feel good in your skin again.
WE SEE YOU. WE UNDERSTAND YOUR FRUSTRATION WITH FINDING SOLUTIONS FOR MELASMA.
WE’RE HERE TO HELP.
BOOK A CONSULTATION WITH AN EXPERIENCED AUSTRALIAN DOCTOR TODAY TO DISCUSS YOUR SKIN TREATMENT OPTIONS: CLICK HERE
REFERENCES:
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009 Oct 20;120(16):1640-5. doi: 10.1161/CIRCULATIONAHA.109.192644. Epub 2009 Oct 5. PMID: 19805654.
Australian College of Rural and Remote Medicine. (2024). Melasma management in primary care. The Australian Journal of General Practice, 53(12).
D’Elia, M., Cassiano, D., Espósito, A., & Miot, H. (2022). Concerning the characterization of metabolic syndrome in epidemiologic studies. Comments on “metabolic syndrome in melasma: A case–control study”. Journal of Cosmetic Dermatology, 21. https://doi.org/10.1111/jocd.15347.
Karaali, M. (2022). Retracted: Metabolic Syndrome in Melasma: A case‐control study. Journal of Cosmetic Dermatology, 21. https://doi.org/10.1111/jocd.15076.
Resnik S. Melasma Induced by Oral Contraceptive Drugs. JAMA. 1967;199(9):601–605. doi:10.1001/jama.1967.03120090043007
Castanedo-Cazares JP, Hernandez-Blanco D, Carlos-Ortega B, Fuentes-Ahumada C, Torres-Álvarez B. Near-visible light and UV photoprotection in the treatment of melasma: a double-blind randomized trial. Photodermatol Photoimmunol Photomed. 2014 Feb;30(1):35-42. PMID: 24313385.
Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, Nageotte O, Doss N. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010 Sep;24(9):1060-9. PMID: 20202051.
Handel A, Miot L, & Miot H(2014). Melasma: a clinical and epidemiological review. Anais brasileiros de dermatologia, 89(5), 771–782. https://doi.org/10.1590/abd1806-4841.20143063
Hassan S, Zhou XA. Drug-Induced Pigmentation. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542253
Hexsel D, Rodrigues TC, Dal’Forno T, Zechmeister-Prado D, Lima MM. Melasma and pregnancy in southern Brazil. J Eur Acad Dermatol Venereol. 2009 Mar;23(3):367-8. PMID: 18631207.
Hill RC, Stubblefield O, Lipner SR. Melasma Risk Factors: A Matched Cohort Study Using Data From the All of Us Research Program. Cutis. 2024 Sep;114(3):90-92. PMID: 39413320.
Liu, Z., & Fu, W. (2009). Relationship between melasma and ultraviolet radiation. International Journal of Dermatology and Venereology, 35, 196-198. https://doi.org/10.3760/CMA.J.ISSN.1673-4173.2009.03.027.
Mahmood, K., M. Nadeem, S. Aman, A. Hameed, and A. Kazmi. 2016. “Role of Estrogen, Progesterone and Prolactin in the Etiopathogenesis of Melasma in Females.” Journal of Pakistan Association of Dermatology21:241–47.
Moin A, Jabery Z, Fallah N. Prevalence and awareness of melasma during pregnancy. Int J Dermatol. 2006 Mar;45(3):285-8. PMID: 16533230.
Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967 Feb 27;199(9):601-5. PMID: 6071249.
Stančáková, Alena, and Markku Laakso. 2014. Genetics of Metabolic Syndrome. Reviews in Endocrine & Metabolic Disorders 15 (4): 243–52.
Wong RC, Ellis CN. (1989). Physiologic skin changes in pregnancy. Semin Dermatol. Mar;8(1):7-11. PMID: 2701710.
World Health Organization (WHO). (2000). Obesity: Preventing and managing the global epidemic (WHO Technical Report Series, No. 894). World Health Organization. https://pubmed.ncbi.nlm.nih.gov/11234459/
Zhang, X., Chen, Y., Yang, H., Ding, H., Cai, P., Ge, Y., Zheng, H., Sun, X., Yang, Y., Li, X., & Lin, T. (2024). Plasma Metabolomics Indicates Potential Biomarkers and Abnormal Metabolic Pathways in Female Melasma Patients. Annals of Dermatology, 36, 300 – 309. https://doi.org/10.5021/ad.23.141








