

Written by Qr8 Founder Dr Michele Squire PhD
Perimenopause and menopause—the hormonal transition periods where ovarian function declines, leading to reduced levels of oestrogen, progesterone, and testosterone—bring about significant changes to the skin. Much like puberty or pregnancy, menopause is a natural physiological process, yet it remains clouded by misinformation, pseudoscience, and a surge of supplements promising miraculous results but without any scientific evidence that they work.
Oestrogen production peaks around age 30, but many women won’t notice the symptoms of reduced oestrogen in perimenopause (changes in cycle length and flow) until their 40s, around 10 years prior to menopause (the point at which menstrual bleeding has ceased for 1 year).until perimenopause. With life expectancy increasing, women can now spend up to one-third of their lives in post-menopause, managing the lasting impact of declining oestrogen levels on their health, including their skin.
In this article, we explore how oestrogen influences skin health and provide evidence-based skincare solutions for menopausal and perimenopausal women in Australia.
The Relationship Between Oestrogen and Skin
Oestrogen (which is actually a group of hormones – 17β-oestradiol, oestrone, and oestriol – collectively referred to as ‘oestrogens’) primarily function as signalling molecules throughout the body, binding to receptors in various body organs to assist in their optimal function. Oestrogen, especially in decline, affects all these tissues differently.
Oestrogen also plays a major role in skin health. In the face of changes to other organs, skin and aesthetic concerns may seem frivolous – but the changes in skin are the most visible, and it can be difficult to come to terms with these changes in our visible appearance, affecting self-esteem and quality of life.
In skin, oestrogen plays a part in a wide range of beneficial/protective roles. It binds to specialised receptors in skin and:
- Increases blood flow, ensuring optimal delivery of nutrients to skin cells
- Stimulates skin cell proliferation and receptor expression (less oestrogen = fewer receptors)
- Maintains telomere length, delaying cell aging and promoting skin rejuvenation
- Enhances hyaluronic acid, collagen, and elastin production, increasing skin thickness and hydration
- Inhibits enzymes that break down collagen, preventing premature aging
- Promotes wound healing and strengthens the skin barrier
- Acts as an antioxidant, protecting against oxidative stress from sun exposure (‘photoaging’ is the rough, dry, deeply wrinkled, saggy skin with uneven texture and tone that results from chronic sun exposure – more about that here)
Oestrogen also stimulates the hair follicle for hair growth so female pattern hair loss (‘androgenetic alopecia’) is also an issue that can start in perimenopause.
Our doctors can help prevent hair loss and regrow thinning hair. Book a video appointment to discuss treatment HERE >>
How Skin Changes in Perimenopause & Menopause
As women start their menopause transition in their 40s, reduced circulating oestrogen means there is less of it to bind skin receptors, leading to changes in the skin’s function and appearance. These changes are more obvious in facial skin as cells in this area has more oestrogen receptors than other areas of the body. As you will see, these are not just ‘appearance based’ concerns, but issues of skin health and function.
These changes are:
Dry, Dull Skin
- Reduced hyaluronic acid production and sebum output result in dry, lackluster skin.
- Skin loses its ability to hold moisture, leading to increased sensitivity and a weakened skin barrier.
- Poor circulation contributes to dullness and reduced skin renewal.
Fragile Skin
Nearly every cell involved in skin repair is influenced by oestrogen. Declining levels impair wound healing, making post-procedural recovery slower and increasing sensitivity to treatments like microneedling, laser therapy, and dermabrasion.
Skin Laxity, Sagging, and Wrinkles
30% of skin’s dermal collagen content is lost in the first 5 postmenopausal years, with an average decline of 2% per year over a period of 15 years. This alters the skin’s mechanical properties, and results in skin that is thinner and weaker. These collagen changes also trigger degenerative changes in the skin’s elastic fibres, making skin less plump and ‘bouncy’, and more prone to wrinkle formation.
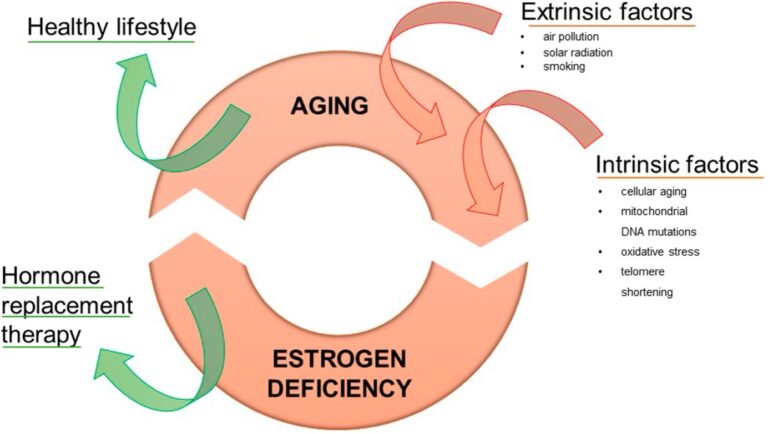
Combine this with the fact that skin aging occurs at different rates due to external factors such as pollution, diet, smoking and sun exposure. The most of important of these is the sun’s UV radiation and visible light (blue-violet) wavelengths, which upregulate hormones in the skin that break down collagen and elastin, and cause oxidative damage (known as ‘photodamage’). This exacerbates skin laxity, sagging, deeper wrinkles, pigmentation and skin lesions such as actinic keratoses, and melanoma/non-melanoma lesions (see the diagram below).
What are effective treatments for menopausal skin changes?
1. Chat with your doctor about Hormone Replacement Therapy (HRT)
There is robust scientific evidence that hormone replacement therapy can reverse many of the skin issues associated with hormonal ageing, along with many other symptoms of menopause. There are equally a lot of myths and misinformation about HRT (including some designed to sell you something more expensive and unnecessary), so it’s definitely something to discuss with your doctor to make an informed choice about whether HRT is right for you.
2. Don’t get conned into supplements
With the rise of the menopause movement, there will always be celebrities, salespeople (and even doctors!) who see an opportunity to exploit your distress. Every corner of the internet is filled with supplements promising to alleviate your hormonal symptoms. But buyer beware: some of the most common menopause supplement ingredients (black cohosh and turmeric) are suspected of causing liver failure, even though based on all available evidence, black cohosh has no evidence for treating menopause symptoms anyway. If you’re suffering from menopause symptoms we would always recommend seeing a womens’ health doctor and dietitian for personalised advice.
Skincare is no different – there is no end of ‘anti-aging’ skincare and supplements directed towards menopausal women. Don’t be fooled though – most of these provide no more support than plain moisturiser and sunscreen, and often come at a very high price point (read further for our skincare advice about what works, and what doesn’t).
There is sound scientific evidence that low molecular weight collagen peptide supplements stimulate increased collagen, elastin and hyaluronic acid production in the skin, plumping out wrinkles and increasing the skin’s hydration and elasticity levels in the process. But this needs to be taken consistently, at the correct dose of at least 3mg/day, and used in combination with evidence-based skin treatments and proper use of sunscreen. Taking a collagen supplement on its own, without any of these things, will not produce miracles.
3. Then, think about your basic skincare routine
The best skincare products for oestrogen-deprived skin are plain, fragrance-free and nourishing for dry, fragile skin. Keeping things simple will also reduce your chances of having a reaction. Although the visible signs of oestrogen deprivation can be distressing, it’s important to make informed choices about your skincare – it’s definitely NOT the time to start experimenting with a complicated skincare routine!
Examples of these products include: a gentle, fragrance-free cleanser and moisturiser that respects and improves the skin barrier without irritation, and using sun protection properly (a little bit of sunscreen is NOT better than none at all). If you are a Qr8 patient, our Skincare Support Team will help you choose the best skincare products for your skin.
And by all means ignore the myth that drinking water improves dry skin. Drinking water (above and beyond your body’s thirst signals) does nothing for skin – but it does make you wee more!
4. Add in evidence-based anti-aging skincare ingredients
Prescription-strength retinoids combined with proper use of a high SPF, broad spectrum (especially UVA-1 protecting) sunscreen, are the only evidence-based anti-aging topical treatments that can stimulate skin cell proliferation, increase HA, elastin & collagen synthesis, reduce collagen breakdown, increase blood flow, promote changes in the skin that help with wound healing and repair of sun damage, and minimise wrinkle formation. Glycolic acid has some evidence that it can increase skin thickness, but not to the same extent as a retinoid.
When your skin is accustomed to regular use of retinoids (aim for daily use of the highest strength your skin can tolerate – this differs between people, and our Skincare Support Team will help you reach this target as quickly and safely as possible), you can then add in other minor players like vitamin C (in the form of L-ascorbic acid) to protect against oxidative damage with your sunscreen, and glycolic acid.
What About Topical Oestrogen Creams?
There is some evidence that they can increase skin collagen and hydration, but the evidence is conflicting, and they are not suitable for everyone.
Watch Dr Michele discuss these creams HERE >>
The Growing Focus on Menopausal Skincare
The beauty industry has long ignored women over 40, but that is changing. In Australia, women over 45 represent a significant consumer demographic with considerable purchasing power. By 2025, over 1 billion women worldwide will be in menopause—representing 12% of the global population.
Menopausal skincare isn’t just about aesthetics; it’s about overall health and well-being. Educating yourself on science-backed treatments ensures informed decision-making and the best possible care for your skin during this transition.
WE SEE YOU. WE UNDERSTAND YOUR FRUSTRATION WITH FINDING SOLUTIONS FOR SKIN DURING AND AFTER MENOPAUSE.
WE’RE HERE TO HELP.
BOOK A CONSULTATION WITH AN EXPERIENCED AUSTRALIAN DOCTOR TODAY TO DISCUSS YOUR SKIN TREATMENT OPTIONS: CLICK HERE
REFERENCES:
Rosenthal MS. The Wiley Protocol: an analysis of ethical issues. Menopause. 2008 Sep-Oct;15(5):1014-22. PMID: 18551081.
Merzel Šabović EK, Kocjan T, Zalaudek I. Treatment of menopausal skin – A narrative review of existing treatments, controversies, and future perspectives. Post Reprod Health. 2024 Jun;30(2):85-94. PMID: 38379168.
El Mohtadi M, Whitehead K, Dempsey-Hibbert N, Belboul A, Ashworth J. Estrogen deficiency – a central paradigm in age-related impaired healing? EXCLI J. 2021 Jan 11;20:99-116. PMID: 33510594.
Zomer HD, Cooke PS. Targeting estrogen signaling and biosynthesis for aged skin repair. Front Physiol. 2023 Oct 31;14:1281071. PMID: 38028803.
Rzepecki AK, Murase JE, Juran R, Fabi SG, McLellan BN. Estrogen-deficient skin: The role of topical therapy. Int J Womens Dermatol. 2019 Mar 15;5(2):85-90. PMID: 30997378.
Silva LA, Ferraz Carbonel AA, de Moraes ARB, Simões RS, Sasso GRDS, Goes L, Nunes W, Simões MJ, Patriarca MT. Collagen concentration on the facial skin of postmenopausal women after topical treatment with estradiol and genistein: a randomized double-blind controlled trial. Gynecol Endocrinol. 2017 Nov;33(11):845-848. PMID: 28508697.
Moraes AB, Haidar MA, Soares Júnior JM, Simões MJ, Baracat EC, Patriarca MT. The effects of topical isoflavones on postmenopausal skin: double-blind and randomized clinical trial of efficacy. Eur J Obstet Gynecol Reprod Biol. 2009 Oct;146(2):188-92. PMID: 19450919.
Patriarca MT, Barbosa de Moraes AR, Nader HB, Petri V, Martins JR, Gomes RC, Soares JM Jr. Hyaluronic acid concentration in postmenopausal facial skin after topical estradiol and genistein treatment: a double-blind, randomized clinical trial of efficacy. Menopause. 2013 Mar;20(3):336-41. PMID: 23435032.
Merzel Šabović EK, Kocjan T, Zalaudek I. Treatment of menopausal skin – A narrative review of existing treatments, controversies, and future perspectives. Post Reprod Health. 2024 Jun;30(2):85-94. PMID: 38379168.








